At the Forefront of the Pandemic
From vaccine development to mental health apps, our researchers have stepped up to help

Faculty, students and staff in the School of Engineering and Applied Sciences are collaborating with colleagues across the University, the region and the world, sharing their expertise to address critical issues related to the pandemic.
Here we present some of our ongoing research initiatives and results, as well as a few examples of other ways that the engineering and applied sciences community has stepped up to help.
Featured COVID-19 Research & Initiatives
More Effective Vaccines

Biomedical engineer Jonathan Lovell is the lead investigator of a research team that has discovered a technique to increase the effectiveness of vaccines against the novel coronavirus. Lovell’s team had previously developed a technology to convert small, purified proteins into particles through the use of liposomes, or small nanoparticles formed from naturally-occurring fatty components. In the new study, the researchers included a special lipid within the liposomes called cobalt-porphyrin-phospholipid, or CoPoP, which enables the RBD protein to rapidly bind to the liposomes, forming more nanoparticles that generate an immune response. When laboratory mice and rabbits were immunized with the RBD particles, high antibody levels were induced. Compared to other materials that are combined with the RBD to enhance the immune response, only the approach with particles containing CoPoP gave strong responses. Other vaccine adjuvant technology does not have the capacity to convert the RBD into particle-form. The vaccine is now entering clinical trials in South Korea in partnership with Eubiologics, a South Korean vaccine-maker.
The paper, “SARS-CoV-2 RBD Neutralizing Antibody Induction is Enhanced by Particulate Vaccination,” was published in Advanced Materials. The study was supported by the National Institutes of Health, and the Facility for Electron Microscopy Research at McGill University.
Making Safer, Reusable Masks
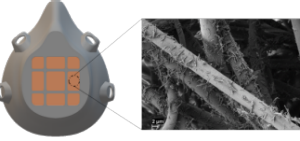
Mark Swihart, professor and chair of the Department of Chemical and Biological Engineering, and his team, in collaboration with UB's Jacobs School of Medicine and Biomedical Sciences and the School of Dental Medicine, has developed materials for antimicrobial masks with possible COVID-19 implications. While face masks are effective in limiting transmission, most medical-grade face masks are not self-sterilized or reusable. Their widespread use consumes tremendous resources and generates a corresponding amount of waste.
Swihart’s team developed a novel material for treating the filtration media used in medical-grade masks to inhibit the growth of microbes. They have produced thin copper@ZIF-8 core-shell nanowires, where ZIF-8 is a zinc-based metal organic framework. When a virus- or bacteria-laden droplet contacts these nanostructures, they slowly release copper and zinc ions, which can kill bacteria and deactivate viruses. These were applied to filtration media by simple dip-coating to uniformly cover the filter fibers. This ensures any deposited droplets will contact the nanomaterial, while requiring miniscule amounts of the material. The filtration performance of the media was maintained or improved. The proposed low-cost and scalable synthesis of Cu@ZIF-8 NWs and straightforward deposition onto filter media has great potential for creating reusable face masks and other medical textiles to reduce disease transmission, resource consumption and environmental impact of waste.
The paper, “Copper@ZIF-8 Core-Shell Nanowires for Reusable Antimicrobial Face Masks,” was published in Advanced Functional Materials.
Discovering Treatments for COVID-19
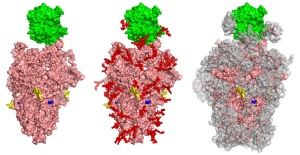
A molecular model of SARS-CoV-2 Spike protein binding to human ACE2.
Sriram Neelamegham, a professor in the Department of Chemical and Biological Engineering, and colleagues are developing molecular strategies to inhibit SARS-CoV-2, the virus that causes COVID-19. The spike protein of this virus has several carbohydrates, known as glycans, attached to it. The overarching goal of the research is to identify weaknesses in viral binding, entry and replication that can be exploited for therapeutic benefit. Their studies have revealed that glycan epitopes expressed on the virus may serve as novel druggable targets. They observed that modifying carbohydrate epitopes using both genetic approaches and small molecules may enable fine-tuning of viral entry into host cells. The small molecule inhibitors they are evaluating represent potential drugs that could be used to ameliorate COVID-19 as well as other viral infections.
The paper, “Inhibition of SARS-CoV-2 viral entry upon blocking N- and O-glycan elaboration,” was published by eLife.
Reducing Worry and Stress in Low Income Neighborhoods

Wenyao Xu is part of a team of UB researchers who are helping adults living in low-income, racial- and ethnic-minority neighborhoods reduce stress due to the COVID-19 pandemic. The $2.5 million award comes from the independent and non-profit Patient-Centered Outcomes Research Institute. The research team will compare a videoconference mindfulness-based stress reduction (MBSR) group intervention to a MBSR mobile app. Both approaches seek to reduce worry among adults living in these areas who have limited or reduced access to mental health care, particularly due to the pandemic. Xu, an associate professor in the Department of Computer Science and Engineering, is leading the technical team in the development of the app. The app will provide an innovative alternative to current mental health care. It is more accessible, portable and cost-effective, and lowers the barriers to treatment. The project is led by the UB School of Nursing, and the contract is one of seven awarded by the Institute nationwide through a special COVID-19-targeted funding announcement.
Wastewater Surveillance for COVID-19

Ian Bradley, an assistant professor in the Department of Civil, Structural, and Environmental Engineering and the RENEW Institute, is leading a pilot program with environmental engineering colleagues Yinyin Ye, assistant professor, and Ning Dai, associate professor, to monitor wastewater from all of the treatment plants located in Erie County, which includes the city of Buffalo. The researchers are working on an analysis of all the data that has been collected since September with the aim to create a public dashboard in collaboration with the Erie County Department of Health and Sewer Authority.
Bradley is also piloting an innovative wastewater surveillance approach to monitor a wide range of viral infections on campus, extending the capacity of current wastewater surveillance techniques that are based on genome detection. The proposed research will involve interdisciplinary collaborations between environmental engineers and analytical chemistry faculty and students to develop methods for detection of viral proteins and levels of antiviral drugs and other pharmaceuticals, such as anti-inflammatory drugs that are used in managing complications of viral infections in wastewater. Yinyin Ye is a co-investigator on the project.
Developing Low-Cost Ventilators

Early in the pandemic, there was a severe shortage of ventilators needed by critically ill COVID-19 patients. In response to this need, a team of engineers and doctors joined forces on a fast prototyping project based on additive manufacturing technology and resources from the open source motion control community. The system is based on a mechanical actuating device that is coupled to a manual Ambu bag. Additive manufacturing technology was used to construct the mechanical ventilator and a mechatronic system was developed to achieve reliability and motion control accuracy. Early tests showed that the system could achieve a respiration rate up to 30 cycles per minute and a maximum pressure of more than 60 cmH2O. Under atmospheric pressure, the delivery volume of each respiration achieved 750 ml, which meets the basic clinical requirement. The team’s first basic functional version was delivered for testing within 72 hours.
As a case study for implementation of fast prototyping technologies with limited resources, the project has great potential to assist the health care community under crisis conditions like the COVID-19 pandemic. The project team includes Chi Zhou, associate professor, and Tianjiao Wang, PhD student, Department of Industrial and Systems Engineering; Ruogang Zhao, associate professor, and Albert Titus, professor and chair, Department of Biomedical Engineering; Sanjay Sethi, chief of pulmonary, critical care and sleep medicine, and Julia Faller, assistant professor of anesthesiology, Jacobs School of Medicine and Biomedical Sciences. It was partially funded by National Science Foundation.
Impact of COVID-19 on Air Pollution in Urban Areas
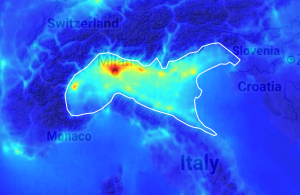
In an effort to learn how air pollution has changed in populated areas of the world, and how these changes might impact the chemistry of the atmosphere in the future, Kang Sun is studying three polluted regions: Southern California, the Jianghan Plain (which includes Wuhan) in China and the Po Valley in Italy, where once-congested streets were made easily navigable by travel restrictions associated with the novel coronavirus. Sun, an assistant professor in the Department of Civil, Structural and Environmental Engineering and the RENEW Institute, is developing a new data-driven framework that combines satellite and meteorological data, that will take NASA satellite assets one step further to quantify the reduction in emissions and their impact on atmospheric chemistry. The resulting framework can eventually be quickly applied to other regions. The project is funded by a $100,000 grant from NASA’s Earth Science Division, through its Rapid Response and Novel Research in Earth Science initiative.
Developing 3-D Printed, Reusable N95-Like Respirators

Most 3D respirators are made of sturdy hard plastic but lack the sealing capability of traditional respirators, which are flexible and designed to form a protective barrier around the face. To address this limitation, Albert Titus, professor and chair of the Department of Biomedical Engineering, is leading a team to design safe, effective and reusable N95-like respirators. The respirators are made from a malleable plastic that requires more expertise to print, and have an opening to insert a filter cut from MERV 15 air filters that are commonly used in hospitals, clean rooms and other environments. An added benefit is that they would be reusable because they could be sanitized after each use.
Another idea is to custom print respirators for a specific person. Either an actual scan from a 3D face scanner or a 3D model of a person’s face from a phone or tablet-camera could be used as the blueprint. The team also designed plans for at least five different respirator sizes that take into consideration typical female and male facial features. This is believed to be unique, as many 3D-printed respirators are based on a one-size-fits-all approach.
The team includes researchers from the Jacobs School of Medicine and Biomedical Sciences, the School of Dental Medicine, and the Sustainable Manufacturing and Advanced Robotic Technologies (SMART) Community of Excellence. They are also working with e-NABLE, an online community that works on 3D-printed prosthetics and other devices, to develop and validate designs that are more comfortable and more communication-friendly.
Improving Air Safety for the Buffalo Philharmonic Orchestra
Francine Battaglia, professor and chair of the Department of Mechanical and Aerospace Engineering, and graduate student Vedant Joshi, are examining COVID-19 safety efforts implemented by the Buffalo Philharmonic Orchestra in Kleinhans Music Hall. Of concern is the spacing between musicians and whether the Plexiglas shields provide sufficient protection to the musicians during performances. The work includes examining a high-denier material to cover the bell of brass instruments to reduce the amount of respiratory aerosols released as an instrument is played.
Modeling the Effectiveness of PPE for Children

Members of the Advanced Simulations for Computing ENergy Transport (ASCENT) Laboratory, led by Francine Battaglia, professor and chair of the Department of Mechanical and Aerospace Engineering, are investigating the protective features of the Little Lives PPE Face Shield™, a commercially available personal protective equipment product designed primarily for children. The team, which includes graduate student Vedant Joshi, is using computational fluid dynamics to numerically model and simulate the fluid flow and track the spread of a virus such as COVID-19. The objective is to determine how air flows around the face shield and how well it prevents the spread of airborne viruses emitted during the wearer’s respiratory processes such as sneezing, coughing and breathing.
Early Detection of COVID-19 at Home
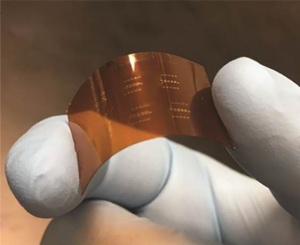
Arindam Sanyal, an assistant professor in the Department of Electrical Engineering, and Jung-Hun Seo, assistant professor in the Department of Materials Design and Innovation, have teamed up with colleagues at Emory University, to develop a solution for early detection and management of COVID-19. The idea is to use wearable bio-sensors to continuously monitor patient physiological signals, such as heart-rate, respiration-rate, blood oxygen content and temperature, together with artificial intelligence (AI) to analyze the sensor data and predict if the wearer has been infected. The multi-modal bio-sensing patch comprises a flexible bio-sensor designed with ultra-thin nanomaterials (<5µm thickness) and embedded AI that continuously analyzes 5-10s frames of sensor data and transmits abnormal segments to a cloud AI model. The cloud AI model performs fusion of multi-modal sensor data and the patient’s electronic medical records to accurately predict if they have been infected.
The preliminary focus of the research is on predicting cardiac events, such as arrhythmia, and sepsis from user physiological signals. The device can predict arrhythmia with 98% accuracy (sensitivity of 0.9) and sepsis with 86% accuracy three hours before onset. The team is now modifying the AI algorithm and the silicon integrated circuit to predict COVID-19 infection, and the immediate anticipated impact is the development of an at-home COVID diagnostic kit that will result in early detection. Successful generalization of the proposed technology may lead to a new frontier of at-home patient-health monitoring devices that can target different bio-markers and allow early screening of preventable diseases, which will improve healthcare quality for all.
Helping the Homeless

Albert Titus, professor and chair of the Department of Biomedical Engineering, was part of a group from UB that donated more than 200 reusable 3D-printed face masks and 100 face shields to the Buffalo City Mission. The masks and face shields were created by UB’s 3D printing group, which formed at the start of the pandemic as a partnership among faculty, staff and students in the School of Dental Medicine, School of Engineering and Applied Sciences and the Jacobs School of Medicine and Biomedical Sciences.
Early in the pandemic, the UB group teamed up with the Buffalo chapter of e-NABLE, the international, open-source 3D printing movement that has stepped up during the pandemic to produce personal protective equipment for communities all over the world. Together, they developed designs and physical prototypes, and published the designs so that anyone could produce the face shields and masks. Approximately 30 UB students and fellows were involved in the project.
Better Materials for Masks

Prathima Nalam, assistant professor in the Department of Materials Design and Innovation, and Anirban Dutta, assistant professor in the Department of Biomedical Engineering, shared their expertise on mask materials with the community group MadeToAid. They suggested some techniques for using common fabrics and other readily available products to improve filtration effectiveness and reduce viral transmission.
MadeToAid’s fabrication and distribution effort is helping to close the PPE need gap, as well as the product quality gap, by bringing together area designers, manufacturers, the DIY community and UB faculty from across the university, including the School of Architecture and Planning, College of Arts and Sciences, and the Community for Global Health Equity.













